May 17, 2020
An analysis of COVID-19 deaths per million population among the 50 states and the District of Columbia shows that there are three areas of the United States bearing the brunt of the virus as of May 17, 2020. Specifically, the eastern seaboard between Washington, DC, and Boston (areas A1, A2, and A3), Louisiana-Mississippi (area B), and Indiana-Illinois (area C) contain 13 of the 15 areas with the highest death rates from COVID-19:
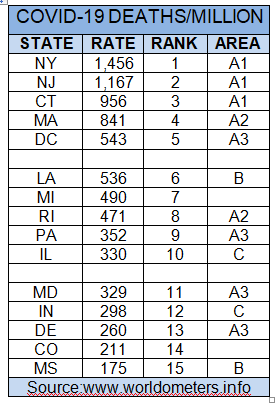 We see that the highest death rates in the country are concentrated in the greater New York area (A1), followed by the greater Boston area (A2). The mid-Atlantic area (A3) is also hard hit. The Louisiana-Mississippi area (B) shows the after-effects of Mardi Gras. Michigan shows a similar death rate, followed by the greater Chicago area. The remaining state on the list is Colorado, ranking 14th. The next 10 states by ranking are Georgia, Ohio, Washington, Minnesota, New Mexico, New Hampshire, Virginia, Nevada, Iowa, and Alabama, with rates ranging from 152 to 100 deaths per million. The remaining 26 states all have current death rates per million below 100. Notable among those states are the 3 most populous states – California (#1, death rate of 83), Texas (#2, 47), and Florida (#3, 92) (New York is #4). Also notable is Hawaii with the lowest death rate per million (12). Hawaii is an island state with an economy heavily dependent on tourism. Hawaii has applied strict rules of entry since early in the pandemic.
We see that the highest death rates in the country are concentrated in the greater New York area (A1), followed by the greater Boston area (A2). The mid-Atlantic area (A3) is also hard hit. The Louisiana-Mississippi area (B) shows the after-effects of Mardi Gras. Michigan shows a similar death rate, followed by the greater Chicago area. The remaining state on the list is Colorado, ranking 14th. The next 10 states by ranking are Georgia, Ohio, Washington, Minnesota, New Mexico, New Hampshire, Virginia, Nevada, Iowa, and Alabama, with rates ranging from 152 to 100 deaths per million. The remaining 26 states all have current death rates per million below 100. Notable among those states are the 3 most populous states – California (#1, death rate of 83), Texas (#2, 47), and Florida (#3, 92) (New York is #4). Also notable is Hawaii with the lowest death rate per million (12). Hawaii is an island state with an economy heavily dependent on tourism. Hawaii has applied strict rules of entry since early in the pandemic.
Viewed another way, areas A, B and C have just over 26% of the US population (87.4 million), but over 70% of the US deaths (64,503 of 90,978) as of May 17, 2020. By comparison, California, Texas, and Florida have just over 27% of the US population (89.9 million) but only 7% of the US deaths (6,522). Almost every state is beginning to re-open, with at most 13 states in compliance with the national guidelines for re-opening (14 days of declining cases).
The incredible virulence of COVID-19 in areas A, B and C make clear the enormous risks if re-opening is not managed according to the by now well-known principles of public health – test, contact trace, and isolate. The public must be prepared not only to comply with but to demand quick action from the appropriate governor to step back from re-opening in any area where cases spike.
UPDATE: August 4, 2020
As almost 3 months have passed, has the above analysis changed significantly? We know that many states outside the top 15 above have had significant case surges, including the three most populous US states mentioned above – California, Texas and Florida. But cases in these states have more predominantly hit younger Americans, who have lower death rates from COVID-19. Here are the 15 states with the highest deaths per million as of August 4, 2020:
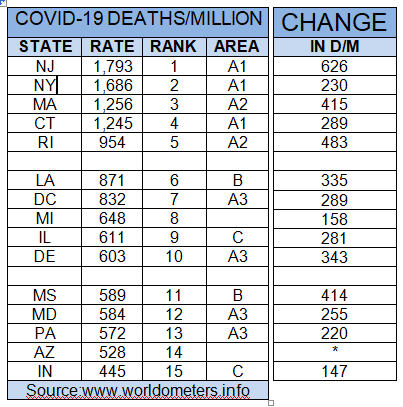 Remarkably, there is only one new state in the table, Arizona, replacing Colorado in 14th place. The 13 states in areas A, B and C all remain in the table, as does Michigan. However, the deaths per million have increased substantially, from 147 (Indiana) to 626 (New Jersey). In two states (Rhode Island and Delaware), deaths per million have more than doubled, while in Mississippi deaths per million have more than tripled. The next 10 states have shifted noticeably from May 17, now Georgia, South Carolina, Florida, Alabama, Colorado, New Mexico, New Hampshire, Ohio, Minnesota, and Iowa), with rates ranging from 369 to 281 deaths per million. The remaining 26 states have death rates at 280 and below, with Utah at 100 deaths per million and only 8 states with death rates below 100. Hawaii remains lowest, at 19 deaths per million. An increase of only 7 deaths per million in this period shows that Hawaii’s strict rules of entry have worked for this island state.
Remarkably, there is only one new state in the table, Arizona, replacing Colorado in 14th place. The 13 states in areas A, B and C all remain in the table, as does Michigan. However, the deaths per million have increased substantially, from 147 (Indiana) to 626 (New Jersey). In two states (Rhode Island and Delaware), deaths per million have more than doubled, while in Mississippi deaths per million have more than tripled. The next 10 states have shifted noticeably from May 17, now Georgia, South Carolina, Florida, Alabama, Colorado, New Mexico, New Hampshire, Ohio, Minnesota, and Iowa), with rates ranging from 369 to 281 deaths per million. The remaining 26 states have death rates at 280 and below, with Utah at 100 deaths per million and only 8 states with death rates below 100. Hawaii remains lowest, at 19 deaths per million. An increase of only 7 deaths per million in this period shows that Hawaii’s strict rules of entry have worked for this island state.
Quite obviously, the US mismanaged re-opening (too early and not in accordance with CDC guidelines) and has lost control of the pandemic, with case rates currently so high that contact tracing and testing has been overwhelmed and is not currently practical in most areas. It remains necessary to develop and distribute adequate testing resources, to prioritize accuracy and quick turn-around of those tests, and to have appropriate contact tracing resources in place everywhere to provide this capability in areas when this again becomes an effective strategy for controlling COVID-19.
